Red Rash on Penis: Causes, Symptoms, and Treatments
Introduction
If you are dealing with a red rash on penis then the problem that you are suffering from is called Balanitis, which means there is an inflammation of the glans penis. This inflammation presents as an itchy red rash covering the glans(head) of the penis. A couple of other quick definitions before we jump into this topic.
Conditions Related to Red Rash on Penis
1. Posthitis
Posthitis means we have an inflammation of the prepuce.
2. Balanoposthitis
Balanoposthitis means we have an inflammation of the glans and of the prepuce.
Posthitis and balanoposthitis occur in uncircumcised males whereas balanitis can be seen in both uncircumcised and circumcised males. For the most part, in clinical practice, everything is kind of clumped together into the term balanitis which means we have inflammation of the glans and the foreskin.
Now we have to keep in mind and we have to remember the normal physiology of the child, if the child is uncircumcised it’s very normal to have a physiological phimosis.
Phimosis
Phimosis means that we can’t retract the foreskin back over the glans. This is normal because we have adhesions that attach the foreskin to the glans early in life. For most people, this is going to separate naturally by 11 years of age, however, it’s still considered normal to have this attachment by 17 years of age, and so long as the patient can urinate properly we don’t need to do anything about this whatsoever.
Etiology of Red Rash on Penis
Now moving on to the etiology of balanitis. The inflammation can be due to Infectious or
Non-infectious causes.
Infectious Causes of Red Rash on Penis
Infectious causes are really going to include:
- Anaerobic infection
- Candida
- Gonorrhea
- Herpes simplex virus/HSV(rare)
- Human Papilloma Virus/HPV(rare)
- Strep infection(Group A or Group B)
Non-Infectious Causes of Red Rash on Penis
The non-infectious causes are going to include:
- Allergy
- Contact dermatitis
- Atopic dermatitis
- Psoriasis
- Drug eruptions
- poor hygiene
Now we will discuss some of the specific etiologies of balanitis one by one.
How Candida Infection causes red rash on penis
Most common in males having a female partner with recurrent candidiasis (Candida albicans is the most common species isolated). It can also be seen in children especially if there’s recent antibiotic use or if he has contact dermatitis. An important thing to keep in mind is that in children the most common cause of balanitis is poor hygiene. Candida infection that results in balanitis can really be the initial presentation of diabetes especially in an otherwise healthy male. So if we have balanitis and this has never occurred before or if we have recurrent balanitis it’s probably a good idea to do a quick glucose check to rule out diabetes.
Bacterial Causes that lead to a red rash on penis
When talking about bacterial causes most common etiologies here are going to be E.coli, Enterococci, Staphylococcus Aureus, and Streptococcus species(groups A and B).
Contact dermatitis and Allergy
Not only can balanitis be due to poor hygiene which means we don’t have the proper cleaning technique, but it can also be due to excessive cleaning. So this excess of cleaning with water and soap is going to irritate and over-dry the glands which can ultimately lead to balanitis. Those with an allergy to latex may have a reaction after condom use.
Drugs that can cause a red rash on penis
Drug eruptions for the most part are going to occur 30 minutes to a few hours after ingesting the medication. Common medications that can cause balanitis include tetracyclines, salicylates, and sedative-hypnotics. Balanitis can be the sole manifestation of a drug eruption.
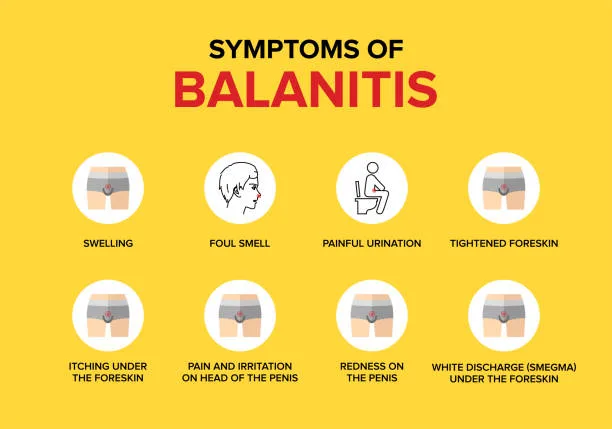

Red Rash on Penis Symptoms?
Let’s get into the signs and symptoms of balanitis. For the most part, patients are going to present with a rash which is going to be present as erythematous papules which can either ulcerate or scale. Patients are going to have pruritis, pain, and tenderness as well. If this is left untreated then this can eventually lead to adhesions, exudates, and edema which can ultimately lead to phimosis and/or paraphimosis. Paraphimosis is a urologic emergency! Paraphimosis means that the foreskin gets trapped behind the glans causing a tourniquet effect.
Balanitis vs Paraphimosis
There are times when paraphimosis can actually be mistaken for balanitis, for example, balanitis presents with an erythematous rash, and paraphimosis can also present with a red
glans and this is because of the constricting effect that occurs with the foreskin constricting behind the glans. What happens is this tourniquet effect is going to reduce venous outflow but
It’s still going to allow for arterial inflow which creates this erythematous glans.
So don’t mistake paraphimosis for balanitis!
Possible Indicators To Rule Out Cause of red rash on penis
Following are some possible indicators to rule out the likely cause of balanitis:
- If we have strep infection anywhere else on the body, skin, or throat, then this is a possible clue to having streptococcus infection as an etiology for balanitis.
- A foul-smelling discharge might clue you into having an anaerobic infection
- Satellite lesions are going to be present with Candida infection
- If we have discharge or ulcers of any kind we have to do an STD workup, especially for chlamydia and gonorrhea
- When doing the physical exam if we palpate the suprapubic area and we have tenderness to palpation, this is where the bladder resides and this might be an indication of a complicated balanitis which means we have urinary retention and these patients ultimately need to be catheterized immediately.
Red Rash on Penis Diagnosis
- The very first thing to do is to exclude the possibility of paraphimosis, as we already have said this is a urological emergency and we really don’t want to miss this diagnosis.
- Once we’ve excluded that possibility, the next step is to do a history and physical examination as we can easily diagnose contact dermatitis, poor hygiene, and candida infection on clinical grounds. These are fairly easy to diagnose and we can go ahead and start the patient on treatment as appropriate
- For those cases that are not quite so clear, we would want to do some laboratory testing including glucose screening to make sure we don’t have diabetes, microscopy, and a chlamydia/gonorrhea screening on certain patients.
- Bacterial cultures really add little to the diagnosis but if required a bacterial culture can also be considered. Also, group A strep culture can be considered As we said streptococcus is a possible etiology as strep can be transmitted orally through oral sex so we have to make sure that that’s not the reason.
Differential Diagnosis
Following are the different possible etiologies that might resemble balanitis:
- Inverse Psoriasis: We should be on the lookout for inverse psoriasis. Inverse psoriasis presents a little bit differently than the classic presentation of psoriasis. This is going to be noted in the intertriginous areas and it’s not going to have the scales or the silver plaques that are going to be normally associated with classic psoriasis
- Scabies, Eczema, and HPV: These types of infections present with papules and balanitis-like symptoms
- Lichen planus: It can occur in the genital area and it’s going to present with violaceous papules over the glans penis
Treatment of red rash on penis
1. Sitz Baths
To reduce the symptoms the patient needs to do sitz baths
2. Hygiene
For proper hygiene, patients should pull the foreskin back and make sure that they clean properly with a Q-tip. Water irrigation especially at the beginning of cleaning plays a big role.
3. Candida Infection
If we have candida infection we’re going to treat it with Topical Azoles (Clotrimazole or Miconazole cream) applied 2 times daily for one to three weeks. We can also use Fluconazole 150 milligrams as a single dose or Nystatin cream as an alternative therapy. But the first line of treatment will be Clotrimazole or Miconazole for one to three weeks.
4. Dermatitis/Allergy
If we have dermatitis or allergy as the possible etiology then we would want to remove the offending agent and then you can also treat it with hydrocortisone 1% cream. We know a lot of people are scared of using steroids especially in this area because it’s supposed to be contraindicated but it’s harmless as cream is going to be less potent than ointments and 1% is a very low dose, hydrocortisone is a very weak topical steroid so you can treat with hydrocortisone 1% cream twice daily but no more than one week as this is considered safe and this help in resolution of symptoms.
5. Drug Eruption
If we have a drug eruption then this is going to be self-limiting as this is going to resolve on its own as soon as the medication is stopped. If the patient has severe symptoms hydrocortisone 1% cream twice a day for no more than one week can be given.
6. Anaerobic Infection
In anaerobic infection, appropriate antibiotics will be used. Options include Metronidazole 500 milligrams twice a day for one week We can also use Augmentin 875/125 twice a day for 7 days. We can also use Clindamycin topical cream applied twice daily for one-week duration
7. Streptococcus Infection
If we’re thinking of group A strep then this is going to be treated exactly like we treat any other type of strep infection. We’re going to use Penicillin for ten days. If there is a history of penicillin allergy then we can substitute it with Cephalosporin, Macrolide, or Clindamycin.
If there is no improvement after four to six weeks of treatment, this is an indication to refer
to the urologist for the appropriate workup and the appropriate treatment.
Word of Caution: Forcing the foreskin back on the penis in phimosis can result in paraphimosis which is an emergency. Paraphimosis acts as a tourniquet reducing venous outflow while simultaneously allowing arterial inflow.
How to Prevent This red rash on penis in the Future?
If we have improper hygiene as the cause of balanitis then the patient should be educated on how to prevent this in the future. If proper hygiene is not maintained then sweat, exfoliated skin, debris, and bacterial organisms are going to overproduce. It’s going to lead to a recurrence so proper hygiene is very important. Patients should also be educated not to over-clean with water and soap as this can lead to atopic dermatitis and this can cause irritation and over-drying of the skin which ultimately leads to balanitis
If you want to learn more about medical topics like these feel free to visit our blog page!!!